Alzheimer’s Drug with Modest Benefits Gets Green Light from FDA Advisers
The drug donanemab slows progression of symptoms in people with early stages of Alzheimer’s disease, but questions linger about the durability of its effect
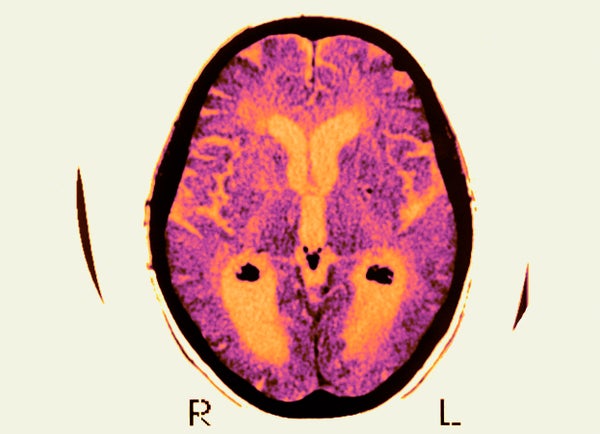
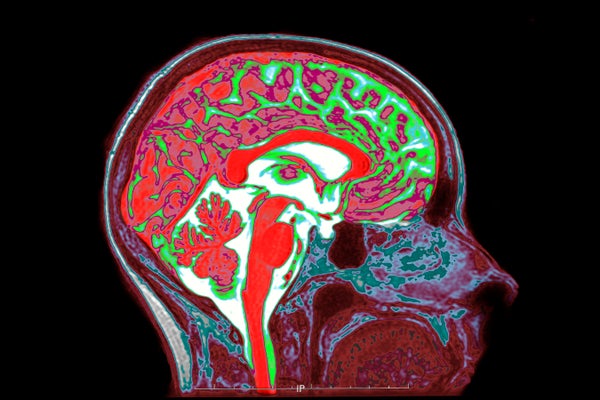
BSIP/UIG Via Getty Images
A drug for Alzheimer’s disease has won unanimous approval from independent scientists advising the US Food and Drug Administration (FDA), bringing the treatment a step closer to use in the clinic.
The drug, donanemab, would be the second on the US market to slow the cognitive decline caused by the disease. But donanemab’s effects are modest, it does not reverse symptoms and the FDA might limit who can take it.
At a 10 June meeting at the FDA’s headquarters in Silver Spring, Maryland, all 11 members of an FDA independent scientific advisory committee voted that donanemab, made by Eli Lilly, based in Indianapolis, Indiana, is effective at treating Alzheimer’s, at least in people in early stages of the disease, and that its benefits outweigh its risks.
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
That an advisory meeting was called at all came as a surprise to many observers, who had expected the FDA to quickly approve donanemab without convening an advisory committee. Instead, the FDA delayed its decision until after the public meeting could be held because of questions about the drug’s efficacy in people with certain markers of Alzheimer’s disease. But, in the end, “it was a very positive meeting”, says neurologist David Knopman at the Mayo Clinic in Rochester, Minnesota, who was not on the committee. “It would have been difficult for someone to object based on the standard of the data.”
Amyloid attacker
Donanemab is an antibody that attacks amyloid, a sticky protein that accumulates in the brains of people with Alzheimer’s disease. In data submitted to the FDA, Eli Lilly reported that the 622 trial participants who received donanemab and completed the trial lost their cognitive abilities more slowly over the study period than did those who received a placebo. However, the drug did not reverse the disease’s progression. Research1,2 shows that donanemab slows symptoms roughly as well as rival drug lecanemab, which also attacks amyloid. Lecanemab is made by the biopharmaceutical companies Eisai in Tokyo and Biogen in Cambridge, Massachusetts.
Unlike previous trials of monoclonal antibodies, Eli Lilly’s study tested only people whose brains contained both amyloid and another protein called tau that is associated with cognitive decline. Donanemab seemed to be more effective in people who had low to moderate tau levels at the start of the trial than in people who had high levels. But the FDA pointed out that the disease might have progressed more slowly in members of the lower-tau group than in those with higher tau levels.
At the meeting, advisory committee members were broadly supportive of the drug. However, some noted that Eli Lilly has little evidence that the drug works in people with no to very little tau. But the committee decided against restricting the drug’s usage on the basis of tau levels, because screening for tau is complex and costly. A screening requirement would prevent an unacceptably high number of people from accessing the drug, the committee decided.
The panel members also expressed concern about amyloid-related imaging abnormalities (ARIA), which are associated with brain bleeding and seizures that which can be fatal. ARIA is thought to occur when the antibodies weaken blood vessels in the brain. Eli Lilly recorded more ARIA-related deaths among people who received the drug than in the placebo group. Lecanemab has also been linked to ARIA, but the increased risk seems to be much higher with donanemab3.
Controversial therapies
The approval is a bright spot for amyloid-targeting Alzheimer’s drugs after numerous controversies. Despite the objections of its advisory committee, the FDA in 2021 approved the first such drug, aducanumab, another medication made by Biogen and Eisai, leading three committee members to resign in protest. A US Congressional investigation later found that that the FDA had improperly guided the manufacturers through the approval process. Many insurers were not convinced of the drug’s efficacy, and most refused to cover it. Biogen stopped making the drug earlier this year. And three people are thought to have died from ARIA-related conditions during clinical trials of lecanemab, sparking an outcry.
The committee convened to evaluate donanemab said that more research is still needed on the drug — for example, on how long people should take it for and its efficacy in people with different levels of tau. Knopman says that it remains to be seen whether the drug’s modest effect will persist for years.
The committee also recommended more research on the drug’s efficacy in people of colour — more than 90% of Eli Lilly’s trial participants were white. And they wanted to see more data on the drug in people who have Down’s syndrome, which raises the risk of Alzheimer’s, or genetic mutations that make them more prone to both Alzheimer’s, and ARIA. Committee member Kathleen Poston, a neurologist at Stanford University Medical Center in California, says scientists need to obtain these data “to make sure that these encouraging findings can be extrapolated to everyone with Alzheimer’s disease”. The FDA’s final decision is expected later this year.
This article is reproduced with permission and was first published on June 10, 2024.